Intramuscular (IM) Injection
Introduction
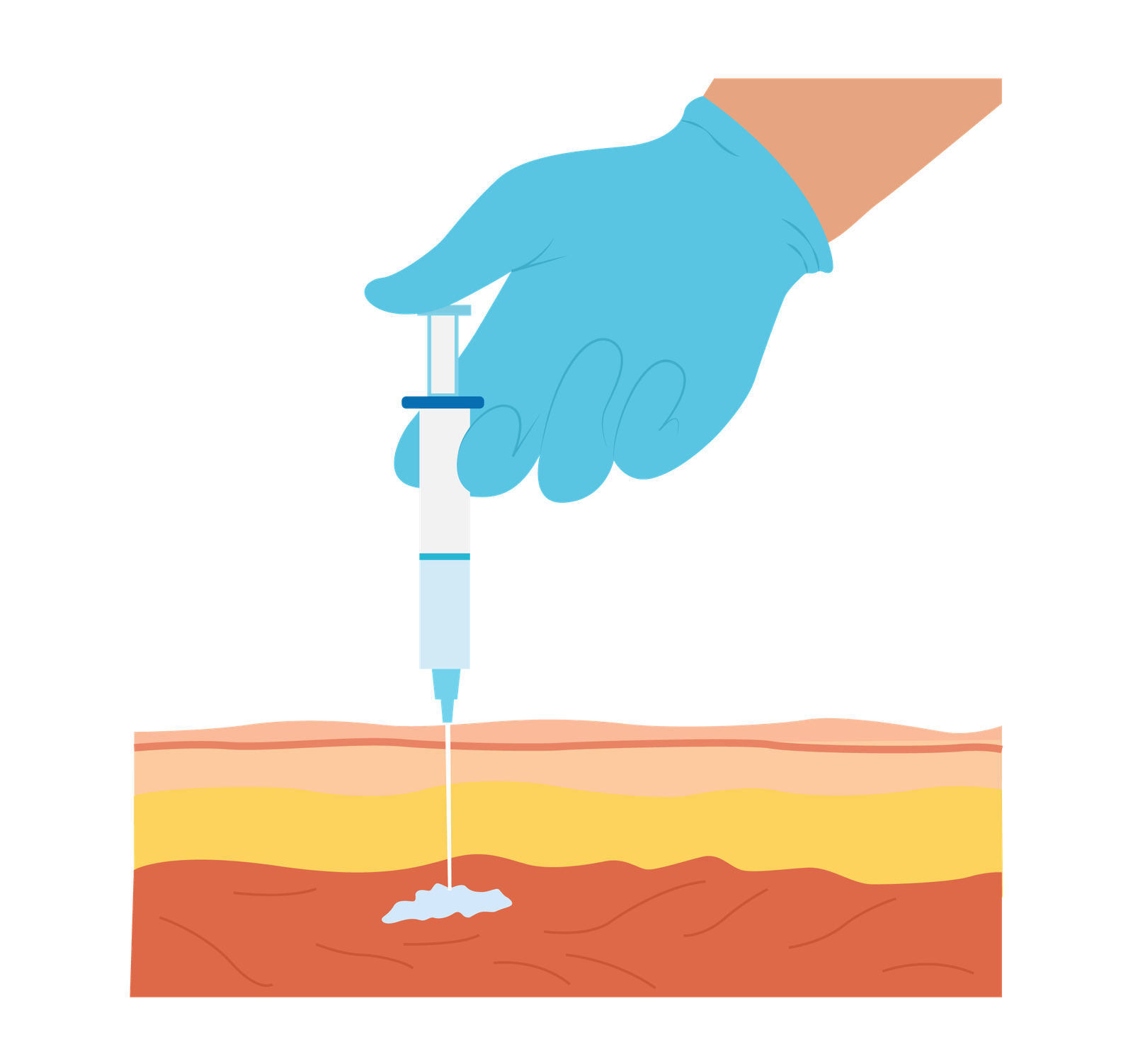
Intramuscular injection (IM) is a route of medication administration that involves delivering medications directly into the muscle tissue. In the prehospital setting, IM injections are frequently used to provide rapid drug delivery when intravenous access is not readily available or contraindicated.
Indications
Medication Administration: IM injections are frequently used to administer medications that require deep tissue penetration, sustained release, or are poorly absorbed through other routes. Examples include vaccines, antibiotics, analgesics, antipsychotics, and hormonal preparations.
In emergency situations where immediate drug delivery is crucial, IM injections are preferred when intravenous access is not readily available or feasible. Medications such as adrenaline for anaphylaxis, naloxone for opioid overdose, and morphine for pain relief can be administered via IM route.
Contraindications
Allergy to the medication being administered via the IM route.
Active infection at or around the injection site. Choose alternative if necessary.
Cautions
Bleeding Disorders – may be at increased risk of bleeding or haematoma formation at the injection site.
Agitated Patients – May be more difficult to achieved accurate site location.
Local Skin Lesions – Significant skin lesions, ulcerations, burns should be avoided as it may worsening the condition of interfere with medication absorption.
Lack of Muscle Mass – Patients with severe muscle wasting or atrophy may not have adequate tissue for proper absorption.
Intramuscular InjectionsComplications
While intramuscular injections (IM) are generally safe and well-tolerated, there are potential complications that can occur.
Pain/Discomfort – It is typically transient and resolves within a short period. Good technique, site selection and insertion angle can help minimise pain.
Bleeding/Hematoma – May cause bleeding at injection site, with formation of a hematoma.
Infection
Tissue Irritation/Damage
Allergic Reaction – Proper assessment of the patient’s allergy history and monitoring for signs of an allergic reaction during and after the injection are important.
Systemic Effects – Some medications administered via IM route can have systemic effects, such as changes in blood pressure, heart rate, or respiratory function.
Injection Sites
When selecting a site for intramuscular injection, there are several factors to consider ensuring safe and effective administration. The specific site chosen may vary depending on the age of the patient, the volume and type of medication being injected, and the size and condition of the muscle. The site should be inspected for signs of inflammations, swelling, and infection.
Deltoid Muscle
Located in the upper arm, the deltoid muscle is often used for smaller volumes of medication (up to 2 mL) in adults and is easily accessible in emergencies.
Expose the patient’s upper arm. Locate the deltoid muscle by feeling for the rounded triangular shape at the upper arm, around 2.5cm (three fingers’ width) below the acromion process (the bony prominence on the shoulder).
Gluteus Maximus Muscle
The gluteus maximus muscle, located in the buttocks, is often used for larger volumes of medication (up to 5 mL) in adults. Caution is needed if this site is chosen as there is a possibility of damaging the sciatic nerve of the superior gluteal artery. Studies have also soon that in obese patients, injections may be adopted by the tissue rather than the muscle, consequently increasing the absorption rate of the drug.
Ask the person receiving the injection to lie on their stomach or side, exposing the upper outer quadrant of the buttock. Locate the injection site by dividing the buttock into four quadrants and selecting the upper outer quadrant.
Ventrogluteal Muscle
The ventrogluteal muscle, located in the hip area that also accesses the gluteus medius muscle, is another site that can be used for intramuscular injections. It is a deep and thick muscle that is relatively free from major nerves and blood vessels. This site is recommended as the primary location for IM injections.
Place the heel of your hand over the greater trochanter (the bony prominence on the hip) with your fingers pointing towards the patient’s head (thumb pointing anteriorly). Your index finger should rest on the anterior superior iliac spine (the bony prominence on the front of the hip). The triangle formed between your index and middle fingers is the target area for the injection.
Vastus Lateralis Muscle
Situated in the lateral part of the thigh, the vastus lateralis muscle is often used for infants, young children, or patients unable to walk. It provides a large muscle mass for injection and is relatively safe.
The vastus lateralis muscle is located on the outer side of the thigh. To find the site, imagine dividing the thigh into thirds both horizontally and vertically. The injection site is in the middle third, on the anterior aspect of the thigh.
Z-Track Technique
The Z-track technique is a method used for administering intramuscular injections to minimize medication leakage and reduce discomfort for the patient. It involves pulling the skin and underlying tissue laterally or downwards, before injecting the medication. This technique is commonly used when administering medications that may cause irritation or staining of the skin.
Applying traction to an aged patient with diminished muscle mass or an underweight patient is not advised; instead, bunch the muscle to guarantee sufficient size before injecting.
The angle of needle entry varies between literature of 72-90 degrees. To ensure that the needle entry is within the range of 72-90 degrees, the needle should be inserted perpendicular to the patient’s body.
Aspiration should be practised to ensure the needle has not been placed in a blood vessel accidentally.
Additionally, ten seconds should be allocated before removing the needle to allow the diffusion of medication into the muscle. On removal, release the pulled skin which limits leakage form the site. Exercising the limb after can assist absorption of the drug as blood flow is increased to the area.
Equipment
-
Syringe
Choose a syringe of appropriate size to accommodate the volume of medication you are administering.
-
Needle
Select a needle suitable for IM injections. The needle length and gauge will depend on factors such as the patient’s age, body size, and the specific medication being administered.
-
Drawing-up Needle
Filters out sub-visible particles of glass, rubber and other residues when drawing up medications from ampoules.
-
Medication
The specific medication to be injected in the IM route.
-
Alcohol Swab
Use alcohol swabs to clean the injection site before the injection. These swabs help disinfect the area, reducing the risk of infection.
-
Gauze
These are used to apply pressure to the injection site after the injection to prevent bleeding.
-
Sharps Container
It is essential to have a designated sharps container for the safe disposal of used needles and syringes. This ensures proper handling and minimizes the risk of accidental needlestick injuries.
-
Gloves
Wearing gloves during the procedure helps maintain proper hygiene and reduces the risk of contamination.
Intramuscular Injection Procedure
Carry out pre-proecdure checks.
Carry out pre-medication checks.
Draw Up Medication
Dispose of drawing up needle immediately after. Attach the injection needle to the syringe with the medication.
Identify an Injection Site
Identify a suitable injection site and position patient to provide optimal assess to the chosen site.
Prepare the Injection Site
Using the alcohol swab in the crosshatch movement for minimum of 20 seconds.
Stabilise the Injection Site
Use the Z-track technique discussed above.
Insert the Needle
Holding the syringe like a dart, pierce the skin perpendicular to the injection site. Insert swiftly, with the bevel facing upwards and leave approximately one-third of the needle exposed.
Aspirate
Check the needle is not placed within a blood vessel. If blood appears, remove and restart process.
Inject the Medication
Once you have confirmed that the needle is properly positioned in the muscle, slowly inject the medication by pushing the plunger of the syringe. Take care to administer the medication at a controlled pace approximately 1ml every 10 seconds.
Withdraw the Needle
After injecting the medication, wait 10 seconds for the medication to disperse evenly then withdraw the needle from the muscle in a smooth and steady motion and place in sharps box.
Release Traction
Release traction to the skin as discussed in the z-track technique above.
Apply Pressure
Use gauze to apply gentle pressure to the injection site.
Dispose & Document
Dispose of all equipment and PPE and wash hands. Record details including chosen site, date and time, complications if any.
Key Points
- Choose the appropriate injection site based on the patient’s age, body size, and the volume of medication. Common IM injection sites include the deltoid muscle, gluteus maximus muscle, vastus lateralis muscle, and ventrogluteal muscle.
- Insert the needle quickly and smoothly into the muscle at the appropriate depth. Aspirate (pull back gently on the plunger) to check for any blood return. If blood appears, withdraw the needle and restart process.
- Administer the medication slowly and steadily to ensure proper distribution and minimize discomfort. Avoid injecting too quickly to reduce the risk of tissue damage or pain.
- Accurately record the details of the injection, including the site, medication administered, dosage, and any adverse reactions or complications.
Bibliography
Gregory, P., & Mursell, I. (2010). Manual of clinical paramedic procedures. Wiley-Blackwell.
Joint Royal Colleges Ambulance Liaison Committee, & Association of Ambulance Chief Executives. (2022). JRCALC Clinical Guidelines 2022. Class Professional Publishing.