Prehospital Drug Administration
Safe prehospital drug administration for emergency carePrehospital drug administration is a critical component of frontline patient care, requiring sound clinical judgement, accurate dosing, and a clear understanding of pharmacology in time-pressured environments. From analgesia and anti-emetics to life-saving emergency medications, prehospital clinicians must deliver drugs safely, effectively, and in line with current guidance.
This resource explores the principles of prehospital drug administration, including indications, routes of administration, safety considerations, and common pitfalls encountered in the out-of-hospital setting. Designed for paramedics, EMTs, ECAs, and first responders, it supports confident decision-making while recognising the unique challenges of autonomous prehospital care.
Prehospital Drug Administration – Articles
Prehospital Drug Administration – Resources
🔗 British National Formulary (BNF)
Authoritative UK medicines reference providing detailed drug information, including indications, dosing, contraindications, and side effects to support safe prehospital medication administration.
📥Coming Soon
📖 Coming Soon
Prehospital Drug Administration – Did You Know?
Drug absorption can be altered in shock
Reduced perfusion in shocked patients can significantly delay or reduce absorption of IM and SC medications, making route selection critical in time-critical care.
Route choice affects onset and safety
Intranasal and intraosseous routes can provide rapid, effective drug delivery when IV access is delayed or impractical, particularly in emergencies.
Weight-based dosing is high risk
Paediatric and bariatric patients are at increased risk of dosing errors, highlighting the importance of accurate weight estimation and dose checking.
Medication errors often occur under pressure
Time-critical decision-making, cognitive overload, and similar drug packaging contribute to prehospital medication errors, even among experienced clinicians.
Governance underpins safe practice
Many prehospital medications are administered under exemptions, PGDs, or local policies rather than prescriptions, requiring clear understanding of scope and governance.
Prehospital Drug Procedures – CPD Reflection Prompts
Reflective practice is a key part of continuing professional development (CPD) and clinical improvement. Use these prompts below to guide your self-reflection on a recent prehospital drug procedures.
Reflect on a recent prehospital drug administration, such as analgesia, anti-emetics, bronchodilators, glucose therapy, or emergency medications:
- jWhat clinical factors influenced your choice of medication, dose, and route of administration?
- jHow did the patient’s physiology, age, weight, or comorbidities affect your decision-making?
- jHow well did your practice align with current guidance, PGDs, exemptions, or local policies?
- jHow effective was the medication, and how was the patient response monitored?
- jWhat challenges did you encounter, such as time pressure, access difficulties, or drug preparation?
- jWhat would you do differently next time to improve safe and effective drug administration?
asdadasd
Consider writing this reflection in your CPD portfolio or ePortfolio using the Gibbs Reflective Cycle or What? So What? Now What? framework. This reflective exercise not only enhances clinical self-awareness but also provides documented evidence of learning that can count towards your annual HCPC CPD requirements. Keeping detailed, structured reflections like this is essential for maintaining your registration and demonstrating safe, effective, and reflective practice as a healthcare professional. This can count toward your annual HCPC CPD requirements.
Prehospital Drug Administration – FAQs
Frequently Asked Questions about Prehospital Drug Administration in Paramedic Practice
What is prehospital drug administration?
Prehospital drug administration refers to the safe preparation and delivery of medications to patients before arrival at hospital. This includes analgesia, anti-emetics, bronchodilators, glucose therapies, cardiac arrest drugs, and other emergency medications used to stabilise patients and improve outcomes in the out-of-hospital setting.
Who can administer drugs in the prehospital setting?
Drug administration in prehospital care depends on role, training, and governance. Paramedics, EMTs, ECAs, and first responders may administer medications under exemptions, Patient Group Directions (PGDs), or local policies, provided they are trained, authorised, and working within their scope of practice.
Do prehospital clinicians prescribe medications?
Most prehospital medications are not prescribed in the traditional sense. Instead, they are administered under legal exemptions, PGDs, or local service policies. Some advanced practitioners may hold independent or supplementary prescribing rights, depending on qualifications and governance arrangements.
How is medication safety maintained in prehospital care?
Medication safety is supported through structured checks, correct patient identification, accurate dose calculation, adherence to guidance, and post-administration monitoring. Cognitive aids, checklists, and team communication play an important role in reducing the risk of error in time-critical environments.
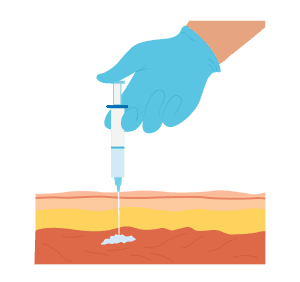
Does the route of administration matter?
Yes. The route of administration significantly affects onset, absorption, and effectiveness. In prehospital care, routes such as intranasal, intravenous, intraosseous, intramuscular, and oral may be selected based on patient condition, access, urgency, and safety considerations.